One of the most common complaints in people who have experienced a COVID-19 infection has been a strange and sometimes long-term loss of smell, a frustrating side-effect.
Depending on various factors, anywhere from 50 to 80 percent of people suffering from COVID-19 can lose their sense of smell.
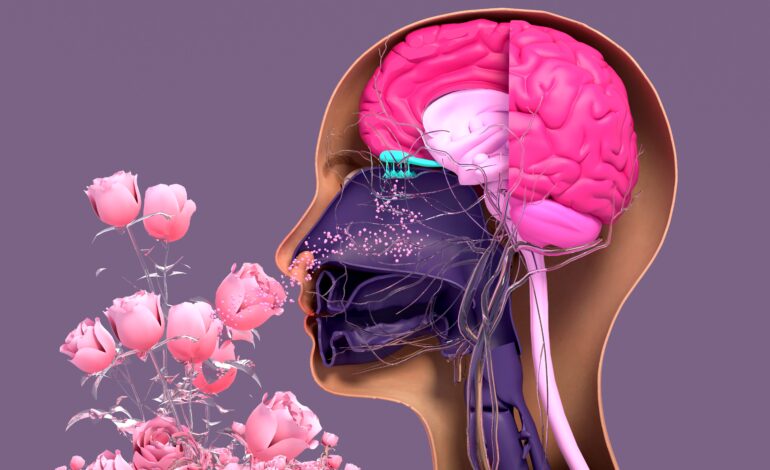
The sense of smell, or olfactory sense, is an essential part of daily life and relies on a complex interplay of nerves, cells and the architecture of the brain itself. Other senses travel through the thalamus — the communication hub of the brain, but smell is transmitted directly to the brain’s emotional center, including the areas responsible for processing emotion and memory.
In fact, brain regions that process smells, memories and emotions are intimately connected.
Specialists say that patients who have lost their sense of smell due to COVID-19, even on a long-term basis, can recover this sense easily by coaxing the brain to recover these connections through therapies and “olfactory training.”
Even after the infection has exited the sinus and respiratory region, some may need this training to re-link smell with memory.
The Arab American News spoke to Henry Ford Health System neurologist Dr. Omar Danoun about the causes of this loss of the sense of smell in COVID-19 patients and what those patients can do to regain their olfactory health.
The nose-smell apparatus
To understand the process of recovery, it is helpful to know how smelling works:

Dr. Omar A Danoun. Photo courtesy: Henry Ford Hospital.
A scent first travels as a chemical particle through the nose and into the olfactory bulb in the brain. There it’s processed into an identifiable scent. Brain cells then carry information about the smell to the almond-shaped region of the brain that processes emotions (the amygdala) and then to the learning and memory center of the brain (the hippocampus).
Research suggests that our brains have 1,000 different receptors for scents, meaning humans have immense smelling potential.
The COVID-19 virus is especially adept at finding a home in the inner structure of the nose and upper respiratory system, specifically to a certain kind of receptor found in the region.
“It’s like a lock and key,” Danoun said. “The lock is the ACE receptors, receptors that naturally occur in the nose, and COVID-19 is the key (grabbing on to the receptor very effectively). So it sticks very well to the inside of the nose, which is why it always affects the nose first.”
Danoun said from there, inflammation sets in as the body fights the virus, which cause further damage to the “nose-smelling apparatus.” This apparatus includes nerve cells that take smell messages to the brain. Those nerves have aids, or support cells, that present smell to it and keep it nourished. Those support cells become affected by the virus, diminishing the power of smell. In patients suffering long-term olfactory damage, the nerve itself gets infected by the virus.
“As a consequence, the nerve function is not optimal and we loose the ability to smell,” he said.
Remembering scents
The good news is that once those cells recover, and they do recover fast, people regain their nose-smell function. This occurs in some 90 percent of people in about one to four weeks after the initial infection.
The process can take some time, as nerve cells don’t regenerate quickly, but they do regenerate and improve. — Dr. Omar Danoun
For others, Danoun said olfactory training or smell therapy acts as physical therapy by repeatedly activating the smell nerves that transmit a smell signal to the brain.
“You bring back smell by putting the nose to work,” he said. “A way to do this is to identify any four smells at home, like lemon, oregano, basil and qahwa, or anything. Smell one item for 25 seconds and then wait for the nose to process it for a minute, go to the next scent and smell for 25 seconds, wait for a minute (and so on). This should be a gentle sniff.”
The patient should then try to imagine the scent of the item, even if they can’t smell it. Do this with the four scents in the morning and at night every day for three months until the smell recovers. For better results, and if the smell does not come back at all in four weeks, Danoun prefers to use essential oils.
“The process can take some time, as nerve cells don’t regenerate quickly, but they do regenerate and improve,” he said.
Danoun recommends using aroma therapy right away when someone loses their sense of smell. If after four to six weeks of natural recovery and/or with therapy, there are no results at all, it’s time to see a doctor. Nasal steroids can help those patients reduce inflammation, as can checking and treating for sinusitis or allergy infections.
Danoun helps patients dealing with other types of olfactory issues as well. He is known nationally for his work with epileptic patients and receives patient referrals from doctors in other states.
During the pandemic, he transformed his living room into a professional-grade studio and uses patient case studies, research and successful treatments in his videos, so he can reach people who can’t get to him or see other doctors and are in need of relief.
The videos are also recorded in Arabic and translated into multiple languages.
Look up Dr. Omar Danoun on YouTube and scroll to the bottom of the English language channel to access his Arabic channel.





Leave a Reply